Our practice follows the American College of Radiology (ACR) recommendations of annual mammography starting at the age of 40 with the exception of other risk factors, such as family history of breast cancer, that may indicate a patient should begin screening early. Your mammography report will include a statement about your breast density, which cannot be determined prior to imaging. Breast density is determined by the radiologist — the doctor reading the mammogram —who assigns each exam to one of the categories.
WHAT DETERMINES BREAST DENSITY?
To understand breast density, you should first understand breast anatomy. For patients assigned female at birth, your natural breast composition will have a mixture of fibroglandular tissue and fatty tissue. These tissues have different cellular structures that will differ how effectively x-rays can pass through them, the variations of which are what create the image. Because the fibroglandular tissue is a denser material, when that tissue overlaps, it can be difficult for the x-rays to pass through the breast to visualize all the tissue types distinctly.
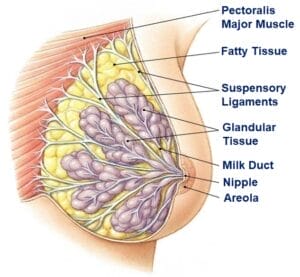 Glandular Tissue – This is a collective term for the breast lobules and ducts.
Glandular Tissue – This is a collective term for the breast lobules and ducts.- Fibrous Tissue – This includes any supportive or connective tissue, such as ligaments and scar tissue.
- Fatty Tissue – This fills the spaces around glands and fibers.
Of course other anatomy in the breast will appear in your images, such as muscles, blood vessels and lymph nodes, but these are not often a contributor to breast density. There are also other naturally occurring breast anomalies that may change the appearance of your breast tissue, such as cysts and fibroadenomas (benign breast tumors), which are also not usually contributory.
WHAT ARE THE BREAST DENSITY CATEGORIES?
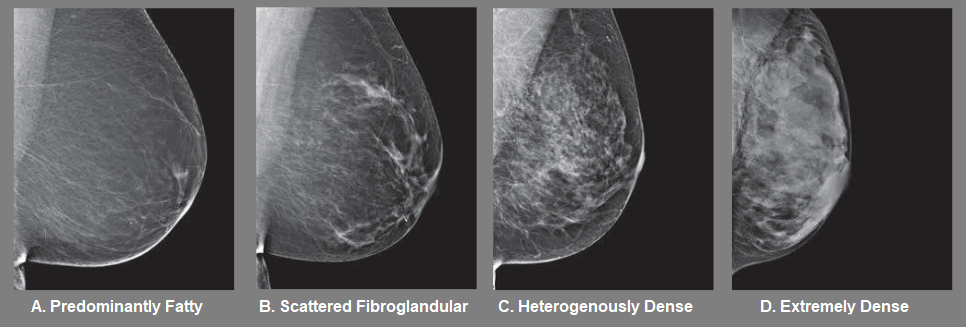
- Predominantly fatty (0-25% Fibroglandular) indicates that the breasts are almost entirely composed of fat. About 1 in 10 women have this result.
- Scattered areas of fibroglandular density (26-50% Fibroglandular) indicates there are some scattered areas of density, but the majority of the breast tissue is fatty. About 4 in 10 women have this result.
- Heterogeneously dense (51-75% Fibroglandular) indicates that there are some areas of fatty tissue, but that the majority of the breast tissue is fibrous or glandular. About 4 in 10 women have this result.
- Extremely dense (76-100% Fibroglandular) indicates that nearly all of the breast tissue is fibrous or glandular. About 1 in 10 women have this result.
If it is determined you have dense breast tissue (Category C or D, or more than 50% Fibroglandular), even if the report indicates no signs of cancer were seen, it is important to know that the nature of dense breast tissue may make it more difficult to see early stages of cancer. Fibrous and glandular tissue appear white on a mammogram, as do some breast masses and cancers, which can be camouflaged by your natural tissue. In contrast, fatty tissue appears almost black on a mammogram, so it’s easier to see a tumor that looks white if most of the breast is more fatty.
MANAGING BREAST HEALTH WITH DENSE BREAST TISSUE
All density categories are normal, and it’s also possible for these categories to change with time, personal factors (weight change, hormone use, etc), technical factors during the mammogram (compression, positioning, etc) or with breast surgery. Your density will be re-evaluated every year during your mammogram, and your report will reflect the most current category and should be the basis for recommendations for your tailored screening strategy with your Columbus ObGyn provider, who will also take into consideration any other relevant risk factors. If found to have dense tissue, you may be offered to get supplemental imaging exams that can be used in conjunction with your mammogram for the most accurate understanding of your breast health.
Annual Screening:
- 3D Mammography (Tomosynthesis)– Despite the appearance of overlapping tissue, most breast cancers can be seen on a mammogram even in women who have dense breast tissue, especially utilizing 3D (tomosynthesis) technology. Tomosynthesis generates a 3-D image of the breast based on x-ray images from multiple angles and can be used to visually separate some of the overlapping tissues. Consistently getting an annual mammogram will provide the radiologist even more information to improve the accuracy of a mammogram, and easily note any changes to a patient’s breast health. Columbus ObGyn has several offices offering this service.
Supplementary Screening:
- Screening Breast Ultrasound/ABUS– This is an ultrasound scan off the entire breast, which is now available in specialty equipment that will provide the radiologist multiple planes of view for comparison. It does not involve radiation and it effectively differentiates tissues of varying densities (fluid vs soft tissue).
- Fast Breast MRI/Abbreviated Breast MRI– This is a condensed version of a MRI that will take images with and without contrast. It does not involve radiation and has the highest sensitivity for detection of the breast screening options.
These will improve the sensitivity of an annual screening, but will not replace the mammogram for multiple reasons, and may not be covered by all insurances. Patients working closely with their provider can help determine which strategy is best for them.







